Targeting Tumor-Associated Macrophages: New Frontiers in Non-Small Cell Lung Cancer Treatment Strategies
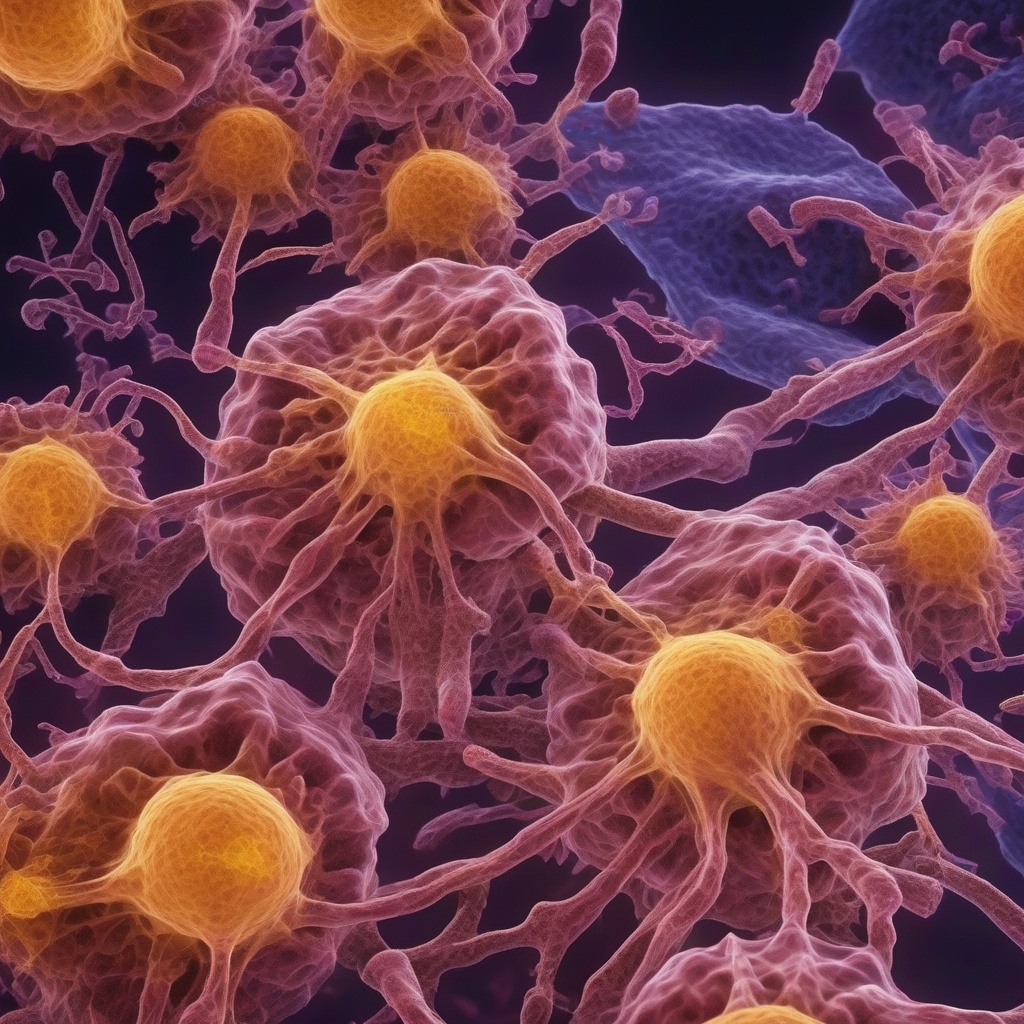
Non-small cell lung cancer (NSCLC) is one of the most common types of lung cancer, accounting for approximately 85% of all lung cancer cases. Despite advances in treatment options, the prognosis for NSCLC patients remains poor, with a five-year survival rate of only 21%. The tumor microenvironment (TME) plays a crucial role in cancer progression and treatment resistance. Tumor-associated macrophages (TAMs) are a key component of the TME, and their targeting has emerged as a promising strategy for cancer therapy.
The Role of Tumor-Associated Macrophages in NSCLC
TAMs are a heterogeneous population of macrophages that infiltrate the tumor tissue. They originate from circulating monocytes and can be polarized into different subtypes, including M1 and M2 macrophages. M1 macrophages are pro-inflammatory and anti-tumorigenic, while M2 macrophages are pro-tumorigenic and immunosuppressive. In NSCLC, TAMs are predominantly of the M2 subtype, which promotes tumor growth, angiogenesis, and metastasis.
TAMs can contribute to NSCLC progression through various mechanisms, including:
- Suppressing anti-tumor immune responses by producing immunosuppressive cytokines, such as TGF-β and IL-10.
- Promoting angiogenesis by producing pro-angiogenic factors, such as VEGF.
- Enhancing tumor cell invasion and metastasis by producing matrix metalloproteinases (MMPs).
- Supporting cancer stem cell maintenance and self-renewal.
Targeting TAMs in NSCLC: Emerging Strategies
Given the critical role of TAMs in NSCLC progression, targeting these cells has become an attractive approach for cancer therapy. Several strategies are being explored to target TAMs in NSCLC, including:
- Monoclonal antibodies: Monoclonal antibodies targeting TAM surface receptors, such as CD47 and CD40, have shown promise in preclinical studies.
- Checkpoint inhibitors: Checkpoint inhibitors, such as PD-1/PD-L1 inhibitors, can also target TAMs and enhance anti-tumor immune responses.
- Cytokine-based therapies: Cytokines, such as IFN-γ and IL-12, can be used to polarize TAMs towards the anti-tumorigenic M1 subtype.
- Gene therapy: Gene therapy approaches, such as RNA interference (RNAi), can be used to selectively target TAMs and inhibit their pro-tumorigenic functions.
Histamine and Histamine Receptors: New Players in TAM-Mediated NSCLC
Recent studies have highlighted the role of histamine and histamine receptors in TAM-mediated NSCLC progression. Histamine is a biogenic amine that plays a crucial role in allergic reactions and inflammation. Histamine receptors, including H1R, H2R, H3R, and H4R, are expressed on various immune cells, including TAMs.
Histamine has been shown to:
- Regulate TAM polarization and function.
- Enhance angiogenesis and tumor growth.
- Suppress anti-tumor immune responses.
Targeting histamine receptors has emerged as a promising strategy for NSCLC therapy. For example, H3R antagonists have been shown to inhibit TAM-mediated tumor growth and angiogenesis.
Conclusion
In conclusion, targeting TAMs has emerged as a promising strategy for NSCLC treatment. Understanding the complex interactions between TAMs, histamine, and histamine receptors will be crucial for the development of effective therapeutic strategies. Further research is needed to explore the potential of TAM-targeting therapies in NSCLC, and to translate these findings into clinical practice.
Read more about the role of histamine and histamine receptors in this article.